Key Takeaways
- The gut–brain axis is the two-way connection between your digestive system and your brain.
- Substance use can disrupt digestion, increase stress signals, and make cravings feel stronger.
- An unbalanced gut microbiome may affect mood, stress, and appetite during recovery.
- Blood sugar crashes can trigger intense urges that feel like cravings.
- Small daily habits, such as steady meals, hydration, sleep, and support, can help reduce cravings over time.
Introduction
Cravings can feel sudden. They can hit hard. And they can make you think something is wrong with you. But cravings are not just about willpower. They are often connected to what your body is going through. Your brain is healing, and your nervous system is trying to settle down.
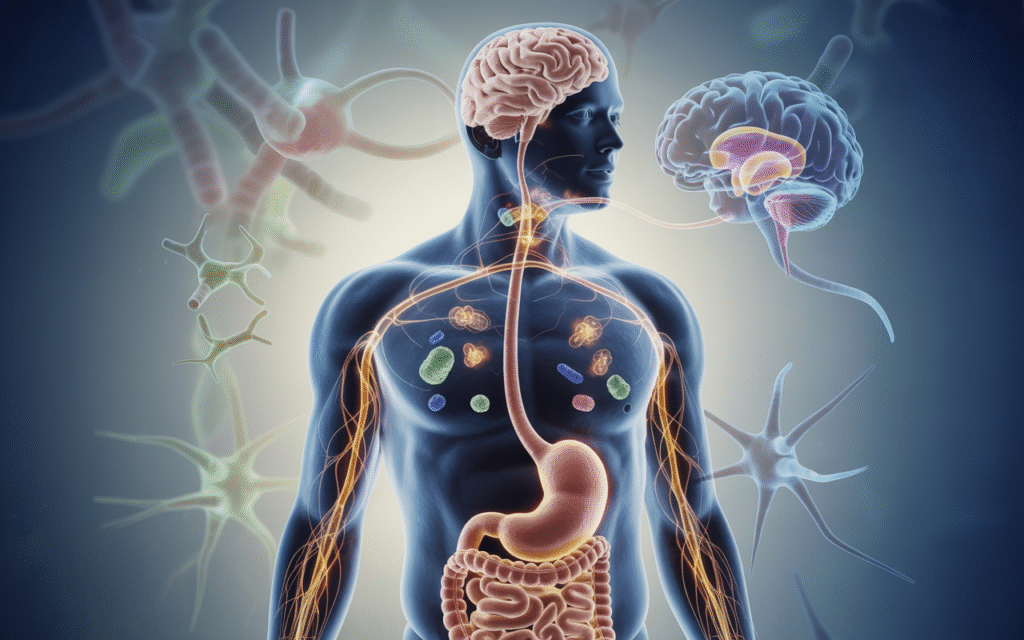
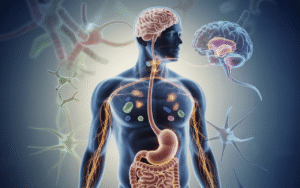
One important part of recovery that people don’t always talk about is digestion. Your stomach and intestines do more than break down food. They send signals to your brain all day long. This connection is called the gut–brain axis. In this article, you’ll learn how digestive health can influence substance cravings. You’ll also learn simple ways to support your gut while your body recovers.
What Is the Gut–Brain Axis? (A Simple Explanation)
The gut–brain axis is a system that helps your gut and brain communicate. It works in both directions.
That means:
- Your brain can affect your stomach
- Your stomach can affect your brain
This is why stress can cause nausea. It’s also why stomach pain can make you feel anxious or upset.
One major pathway in the gut–brain axis is the vagus nerve. This nerve acts like a communication line between your brain and your digestive system. It helps control digestion, heart rate, and even stress response.
Your gut also produces chemicals that influence how you feel. Many people are surprised to learn that digestion plays a role in emotions, focus, and energy. When the gut is irritated or out of balance, the brain can feel the impact.
How Substance Use Can Disrupt Digestive Health
Substance abuse can affect your digestive system in many ways. Some substances irritate the stomach lining. Others change their appetite and sleep. Many can lead to dehydration.
Common digestive issues during active use or early recovery may include:
- Upset stomach
- Nausea
- Stomach cramps
- Diarrhea
- Constipation
- Acid reflux or heartburn
These symptoms are not always dangerous, but they can feel overwhelming. And when your gut feels uncomfortable, your brain may look for relief fast.
That relief can show up as cravings.
During withdrawal and early recovery, your body is also under stress. Stress can slow digestion, increase inflammation, and worsen stomach symptoms. This can create a cycle where discomfort leads to anxiety, and anxiety leads to more discomfort.
The Microbiome and Cravings: What’s the Connection?
Inside your intestines, you have trillions of tiny organisms. This community is called the gut microbiome.
Your microbiome helps with:
- Breaking down food
- Supporting the immune system
- Creating important vitamins
- Helping regulate inflammation
Researchers are also studying how the microbiome may affect mood and behavior. This includes how it may influence cravings. When digestion is out of balance, the brain can receive more stress signals. Your body may feel tense, restless, and “off.” That feeling can make cravings more intense, even if you don’t understand why.
It’s important to keep this realistic, though. Improving gut health can support recovery, but it does not replace treatment. It’s one helpful piece of the full recovery picture.
Blood Sugar, Hunger, and Why Cravings Feel Stronger
Sometimes cravings are not just cravings. Sometimes they’re hungry.
When your blood sugar drops too low, your body goes into a “need energy now” mode. This can cause:
- Shakiness
- Headaches
- Sudden irritability
- Anxiety
- Fatigue
- Strong urges for sugar or quick comfort
For someone in recovery, these feelings can easily blend with cravings. You may feel restless and think, “I need something right now.” That urge can feel just like wanting a substance. This is why steady eating matters. Skipping meals, living off snacks, or eating only sugary foods can cause big blood sugar swings. Those swings can make cravings stronger.
A steadier approach often helps, such as:
- Eating every 3–4 hours
- Having protein with meals
- Adding fiber like oats, beans, or vegetables
- Including healthy fats like nuts or avocado
This is not about dieting. It’s about stability.
Stress, Anxiety, and Stomach Problems That Fuel Urges
Stress can hit your stomach fast. That happens because your brain and gut are closely connected. When you feel stressed, your body releases cortisol, which is a stress hormone. Cortisol can change digestion. It can also affect appetite and sleep.
Under stress, some people feel:
- Tightness in the stomach
- Nausea or “butterflies”
- Loss of appetite
- Sudden hunger
- Bathroom changes
Stress can also make cravings more intense. When your body feels uncomfortable, your brain may remember that substances once offered quick relief. Even if it caused harm later, the brain remembers the short-term “calm.”
This is why recovery needs tools for stress, not just avoidance.
Helpful tools that support both gut and mind include:
- Slow breathing for 60 seconds
- Drinking water and eating a small snack
- Walking for 5–10 minutes
- Grounding skills (naming 5 things you can see, 4 you can touch, etc.)
Small steps can calm the body. And when your body calms down, cravings may reduce.
Warning Signs Your Gut Health May Be Affecting Recovery
Not every stomach issue means something serious. But some signs may mean your digestion is affecting your recovery more than you realize.
Watch for patterns like:
- Cravings that hit after skipping meals
- Mood swings that happen after eating certain foods
- Ongoing bloating or stomach discomfort
- Trouble sleeping because of heartburn or nausea
- Feeling anxious “in your gut” almost every day
- Cravings that spike when you feel stressed or worn down
If you notice these patterns, it doesn’t mean you are failing. It means your body may need support. And if symptoms are severe, it is important to speak to a medical provider.
Gut-Friendly Habits That Can Support Recovery (Realistic Steps)
You don’t need a perfect diet to support recovery. You need steady habits. Here are simple gut-friendly steps that often help people feel more stable.
Start with hydration
Dehydration can make you feel tired, anxious, and foggy. It can also worsen constipation and headaches. Drinking water steadily throughout the day supports digestion and energy.
Aim for steady meals
Try not to go all day without eating. A simple meal plan can be:
- Breakfast
- Lunch
- Dinner
- 1–2 snacks
Choose gentle foods on low appetite days
Early recovery can make appetite feel strange. If big meals feel hard, start small with:
- Soup
- Eggs
- Yogurt
- Oatmeal
- Rice and lean protein
- Bananas or applesauce
Add fiber slowly
Fiber supports gut health, but too much too fast can cause gas and bloating. Slowly add foods like:
- Oats
- Beans
- Whole grains
- Vegetables
Limit what makes symptoms worse
Some people notice more anxiety or stomach upset from:
- Too much caffeine
- Energy drinks
- Greasy foods
- Very spicy foods
You don’t have to remove everything. Just notice what triggers symptoms.
Be careful with supplements
Some people try probiotics, but they’re not for everyone. And not all products are high quality. If you want to try supplements, talk with a healthcare provider first, especially if you have ongoing gut symptoms.
Protect sleep
Sleep affects digestion and cravings. Poor sleep raises stress hormones and lowers your ability to cope. A simple sleep routine same bedtime, less screen time, a calmer evening can make cravings feel more manageable.
How Treatment Helps You Manage Cravings from the Inside Out
Recovery is not only about “stopping.” It’s also about healing what substance use changed inside your body and brain.
Treatment can support cravings by helping you:
- Understand your triggers
- Build a daily structure
- Improve nutrition and hydration habits
- Learn coping skills for stress
- Address anxiety or depression
- Create a relapse prevention plan
Cravings feel powerful when you’re alone with them. Treatment adds support, tools, and a plan. That makes a difference. If cravings feel intense, it doesn’t mean you can’t recover. It means you deserve more support.
Conclusion
Cravings can feel scary. They can feel endless. But they are often a sign that your body is trying to rebalance. The gut–brain axis helps explain why cravings can rise when your digestion is off, your stress is high, or your blood sugar is unstable. When your gut feels better, your brain often feels calmer too.
Small steps like steady meals, hydration, sleep, and stress skills can support your recovery. And professional help can take you further than willpower alone. If you or someone you love needs support right now, call Virtue Recovery Killeen at 866-843-0545 to talk about treatment options.
FAQs
Can gut problems really cause substance cravings?
Gut problems may not “cause” cravings by themselves, but they can make cravings worse. Digestive discomfort, stress signals, and unstable blood sugar can all increase urges.
What foods help reduce cravings during recovery?
Many people do best with steady meals that include protein, fiber, and healthy fats. These help stabilize energy levels and reduce sudden hunger spikes.
Why do cravings get worse at night?
Cravings often rise at night because you may be tired, stressed, hungry, or alone with your thoughts. Evening is also when structure fades, which can make urges feel stronger.
Are probiotics helpful during addiction recovery?
Probiotics may help some people, but they are not right for everyone. It’s best to speak with a healthcare provider before taking supplements.
How long does it take for digestion to improve after quitting substances?
It depends on the person and the substance history. Some people feel better in a few weeks. Others take longer, especially if stress, sleep, or nutrition is still unstable.
When should I see a doctor for gut symptoms in recovery?
Get medical support if you have severe pain, blood in stool, nonstop vomiting, major weight loss, or symptoms that do not improve. Professional care can help you stay safe and stable.
Resources
- National Institutes of Health (NIH) – The Human Microbiome: https://www.nih.gov/news-events/nih-research-matters/human-microbiome
- National Center for Complementary and Integrative Health (NCCIH) – Probiotics and Prebiotics: https://www.nccih.nih.gov/health/probiotics-prebiotics-and-synbiotics
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Digestive Diseases: https://www.niddk.nih.gov/health-information/digestive-diseases
- National Institute on Drug Abuse (NIDA) – Drugs, Brains, and Behavior: The Science of Addiction: https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction
- About the Author
- Latest Posts
Gigi Price holds licenses as a Master Social Worker and Clinical Drug Counselor. She completed her master’s degree in Social Work at Texas State University. Over the last decade, Gigi has been dedicated to utilizing evidence-based practices to enhance patient care and treatment planning, resulting in positive, long-term outcomes for patients and their families. Her passion lies in creating a treatment environment where professionals collaborate to bring about positive change and provide a safe, trustworthy therapeutic experience. Patients can be confident in receiving top-quality care under her leadership.
In her role as the Clinical Director of Virtue Recovery Houston, Gigi conducted research to identify the most effective approaches for treating patients with acute mental health diagnoses, PTSD, and Substance Use Disorder. She then assembled a team of skilled clinicians who could offer various therapeutic modalities, such as Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy
(DBT), Acceptance and Commitment Therapy (ACT), Somatic Exposure, Eye Movement Desensitization and Reprocessing (EMDR), and Cognitive Processing Therapy (CPT). Gigi takes pride in overseeing the development and implementation of Virtue Houston’s Treatment Program, which includes two specialized therapeutic curricula tailored to the unique needs of individuals struggling with mental health issues, addiction, and PTSD.