Key Takeaways
- Neuroinflammation means inflammation in the brain, and it can affect mood, sleep, focus, and cravings.
- Substance use can activate the brain’s immune response and keep it in a state of stress.
- Ongoing inflammation may raise relapse risk by increasing anxiety, low mood, and impulsive behavior.
- Brain healing takes time, but recovery can improve symptoms gradually.
- Treatment helps by supporting the whole person, including sleep, mental health, and long-term relapse prevention.
Introduction
You may stop using drugs or alcohol and still not feel “normal” right away. That can be confusing. It can also feel discouraging. Maybe your mood is up and down. Maybe you feel anxious for no clear reason. Or maybe your cravings still show up, even though you truly want to stay sober.
This is common. And it can have a real biological reason.
One important factor is neuroinflammation, or inflammation within the brain. It can affect how you feel, how you sleep, and how you handle stress. It can even affect how strong cravings feel. In this article, you’ll learn what neuroinflammation is, how substance use can trigger it, and how long-term addiction recovery supports brain healing.
What Is Neuroinflammation? (A Simple Explanation)
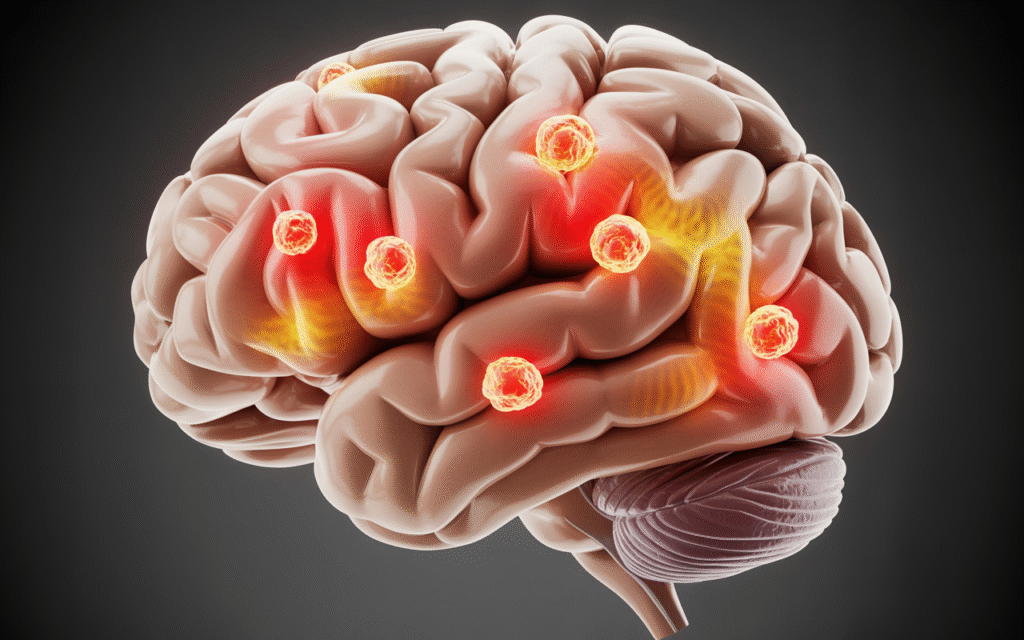
Neuroinflammation is when the brain becomes inflamed due to stress, injury, toxins, infection, or long-term strain.
Inflammation is usually part of healing. It helps the body fight threats. But when inflammation stays active for too long, it can cause problems. Your brain has its own immune cells called microglia. Think of microglia as the brain’s “cleanup team.” They help remove damaged cells and protect the brain.
But when microglia stay activated for a long time, they can cause ongoing swelling and chemical changes. This may affect:
- Mood
- Memory
- Focus
- Sleep
- Stress tolerance
It can also affect the brain’s reward system. That matters in addiction recovery because the reward system plays a big role in cravings.
How Substance Use Triggers Inflammation in the Brain
Substance use can stress the brain in multiple ways. Some substances are toxic to brain tissue over time. Others change brain chemistry and sleep patterns. Many substances also lead to dehydration and poor nutrition, which can add even more stress.
Here are common ways substance use can trigger neuroinflammation:
- Poor sleep and irregular sleep schedules
- Chronic stress and anxiety
- Nutrient deficiencies
- Dehydration
- Repeated withdrawal cycles
- Increased oxidative stress (oxidative stress) in the body and brain
Over time, the brain may start acting like it is always in danger. Even after you stop using, your brain may still stay on high alert for a while. That is one reason recovery can feel hard even after someone quits.
Signs Neuroinflammation May Be Affecting Recovery
Neuroinflammation does not always have one clear sign. It can show up in different ways for different people.
Some common symptoms may include:
- Brain fog or trouble thinking clearly
- Slow memory or poor concentration
- Anxiety that feels constant or intense
- Low mood or feeling emotionally flat
- Irritability or anger over small things
- Sleep issues like insomnia or waking up often
- Feeling tired even after sleeping
- Strong cravings triggered by stress
- Feeling overwhelmed in loud or busy places
These symptoms can also overlap with withdrawal, post-acute withdrawal syndrome (PAWS), and mental health conditions like depression or PTSD. That’s why it helps to get professional support instead of guessing what’s going on.
Neuroinflammation, Cravings, and the Relapse Cycle
Cravings are not just thoughts. Cravings are physical and emotional signals. When the brain is inflamed, stress can feel stronger. The brain can also have a harder time calming down after a trigger.
This can lead to a painful cycle:
- You feel stressed, anxious, or low
- Your brain looks for relief
- A craving shows up
- You feel pressure to escape the discomfort
This does not mean you are weak. It means your brain is still healing. Inflammation may affect the brain’s reward and motivation systems. This can increase impulsive choices, especially when you are tired or stressed.
This is why relapse prevention is not only about saying “no.” It is also about reducing the factors that worsen cravings.
Why Some People Struggle Longer Than Others
Everyone’s recovery timeline is different. Two people can quit the same substance and feel very different months later. Some factors that may slow healing or increase inflammation include:
- Long-term or heavy substance use
- High levels of chronic stress
- A history of trauma
- Co-occurring disorders like anxiety disorders or major depression
- Poor sleep over a long period
- Lack of stable support
- Ongoing medical problems
This is why comparing yourself to others can be harmful. Your brain is healing at its own pace. What matters is staying consistent and getting the right support.
How Long Does Brain Healing Take in Recovery?
Brain healing often happens in phases. Some changes happen quickly. Others take longer. In early recovery, your brain may still be adjusting. Cravings can rise and fall. Mood can feel unstable.
In the weeks and months after quitting, many people notice:
- Improved sleep
- Clearer thinking
- Better emotional control
- Less intense cravings
But for some people, PAWS symptoms can last longer. This does not mean recovery is failing. It means recovery is still in progress. Small improvements matter. Even if it feels slow, healing is still happening.
What Helps Reduce Neuroinflammation During Recovery?
You can’t “force” the brain to heal overnight. But you can support brain recovery through daily habits and professional care. Here are recovery-friendly ways that may help reduce neuroinflammation over time.
Better sleep
Sleep is one of the strongest supports for brain healing. Poor sleep increases inflammation and stress hormones like cortisol.
A basic sleep routine can include:
- Going to bed at the same time
- Avoiding screens close to bedtime
- Keeping the room cool and dark
- Cutting back on caffeine later in the day
Balanced nutrition
Your brain needs fuel to heal. You don’t need a perfect diet. You need steady meals.
Helpful basics include:
- Protein (eggs, chicken, beans)
- Healthy fats (olive oil, nuts, fish)
- Fiber (oats, vegetables, whole grains)
- Stable meal timing to reduce blood sugar crashes
Hydration
Dehydration can make you feel anxious, tired, and foggy. Water supports circulation and digestion, which supports overall recovery.
Gentle movement
Light exercise helps reduce stress and supports mood. Even walking 10 minutes a day can help your nervous system settle.
Stress reduction skills
Stress fuels inflammation. It also triggers cravings.
Simple tools include:
- Slow breathing
- Grounding exercises
- Short walks
- Journaling
- Talking to a trusted support person
Professional support
Therapy and treatment help people build long-term skills. They also help you manage triggers and emotions in a healthier way. In some cases, medications may be recommended by a provider. This can be helpful for depression, anxiety, sleep disorders, or cravings, depending on the person.
When to Get Professional Help
You should never feel like you have to “tough it out” alone. Professional help is important if you have:
- Severe cravings that feel uncontrollable
- Ongoing depression or hopelessness
- Panic attacks
- Thoughts of self-harm
- Frequent relapse or near-relapse episodes
- Sleep problems that are not improving
- Symptoms that make daily life hard
Addiction treatment can help you build a plan that fits your life. It can also help you understand what your brain needs to heal safely. Long-term recovery is not just possible. It is realistic with the right support.
Conclusion
Recovery is not only about quitting drugs or alcohol. It’s also about helping your brain and body heal from what substance use changed. Neuroinflammation may play a role in cravings, mood swings, poor sleep, and brain fog. This can make recovery feel harder than expected.
But brain healing happens step by step. With time, structure, and professional care, many people see real improvement. If you are struggling with cravings or symptoms that won’t go away, help is available. Call Virtue Recovery Killeen at 866-843-0545 to learn about treatment options and support for long-term addiction recovery.
FAQs
What is neuroinflammation in addiction recovery?
Neuroinflammation is inflammation in the brain. It may happen after long-term substance use and can affect mood, cravings, and stress response during recovery.
Can neuroinflammation cause cravings?
It can contribute to cravings by making stress feel stronger and reducing emotional control. Cravings may increase when the brain feels overwhelmed or inflamed.
How long does brain fog last after quitting drugs or alcohol?
Brain fog can last days, weeks, or months, depending on the person. Many people improve gradually with better sleep, nutrition, and treatment support.
Does stress make neuroinflammation worse?
Yes. High stress can increase inflammation and raise cortisol, which may worsen anxiety, sleep problems, and cravings.
Can diet and sleep help the brain heal after addiction?
Yes. Sleep and steady nutrition can support the brain’s repair process and help reduce symptoms over time.
When should I get treatment for long-term recovery symptoms?
If symptoms are severe, lasting, or raising relapse risk, it’s time to get support. Treatment can help you manage cravings and build a stable recovery plan.
Resources
- National Institute on Drug Abuse (NIDA) – Drugs, Brains, and Behavior: The Science of Addiction (NIH): https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction
- National Institute of Neurological Disorders and Stroke (NINDS) – Brain Basics and Neurological Health: https://www.ninds.nih.gov/health-information
- PubMed (NIH) – Neuroinflammation research overview (search portal): https://pubmed.ncbi.nlm.nih.gov/
- National Institutes of Health (NIH) – Brain and Recovery Research Updates: https://www.nih.gov/
- About the Author
- Latest Posts
Gigi Price holds licenses as a Master Social Worker and Clinical Drug Counselor. She completed her master’s degree in Social Work at Texas State University. Over the last decade, Gigi has been dedicated to utilizing evidence-based practices to enhance patient care and treatment planning, resulting in positive, long-term outcomes for patients and their families. Her passion lies in creating a treatment environment where professionals collaborate to bring about positive change and provide a safe, trustworthy therapeutic experience. Patients can be confident in receiving top-quality care under her leadership.
In her role as the Clinical Director of Virtue Recovery Houston, Gigi conducted research to identify the most effective approaches for treating patients with acute mental health diagnoses, PTSD, and Substance Use Disorder. She then assembled a team of skilled clinicians who could offer various therapeutic modalities, such as Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy
(DBT), Acceptance and Commitment Therapy (ACT), Somatic Exposure, Eye Movement Desensitization and Reprocessing (EMDR), and Cognitive Processing Therapy (CPT). Gigi takes pride in overseeing the development and implementation of Virtue Houston’s Treatment Program, which includes two specialized therapeutic curricula tailored to the unique needs of individuals struggling with mental health issues, addiction, and PTSD.