Summary
Combining blood thinners with alcohol can lead to serious health complications, including an increased risk of bleeding and interference with the medication’s effectiveness. Understanding how these substances interact and the potential risks involved is crucial for anyone taking blood thinners like warfarin, rivaroxaban, or aspirin. This article explores these risks and provides safety tips to help manage your health effectively.
Key Takeaways
- Overview of Blood Thinners and Their Purpose: Blood thinners are medications used to prevent blood clots and improve blood flow in patients with conditions such as atrial fibrillation or those at risk of a heart attack or stroke.
- Risks Associated with Combining Blood Thinners and Alcohol: Alcohol use can increase the risk of bleeding and interfere with the effectiveness of blood thinners, leading to potential health complications.
- Types of Blood Thinners and Their Interactions with Alcohol: Different blood thinners like warfarin, rivaroxaban, and aspirin interact with alcohol in unique ways, each carrying specific risks.
- Symptoms and Warning Signs of Complications: Recognizing signs of increased bleeding and alcohol misuse is essential for those combining these substances.
- Safety Tips for Those Taking Blood Thinners and Consuming Alcohol: Consulting a doctor before drinking, moderating alcohol consumption, and monitoring health are critical steps to manage these interactions safely.
Introduction
Blood thinners are crucial medications for preventing blood clots and ensuring proper blood flow in individuals with various health conditions. However, combining these medications with alcohol can pose significant risks. Understanding these risks and knowing how to manage them is essential for anyone taking blood thinners and considering alcohol consumption.
Understanding Blood Thinners
What are Blood Thinners?
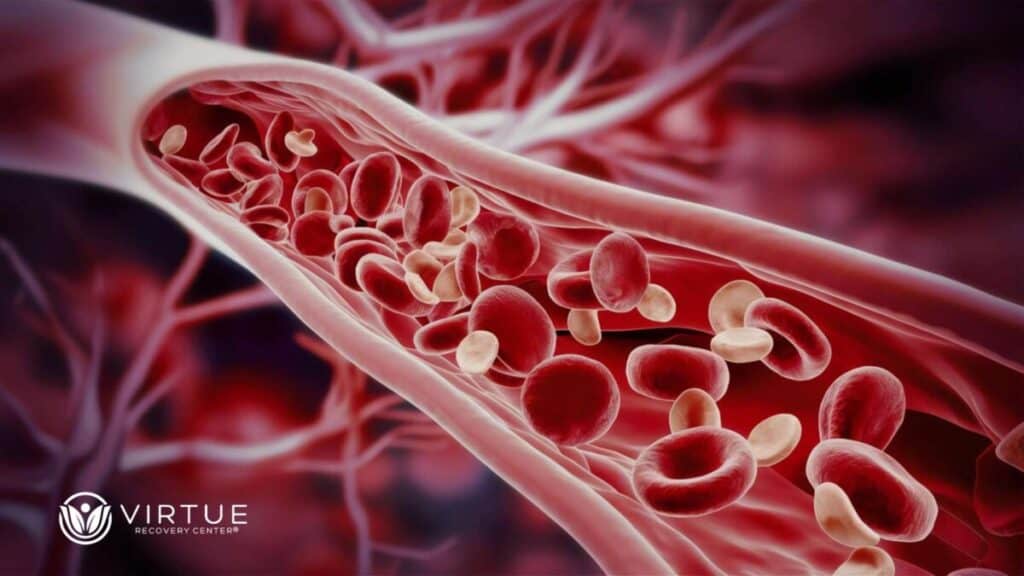
Blood thinners are medications designed to prevent blood clots from forming and to maintain smooth blood flow through the blood vessels. Common types of blood thinners include warfarin, rivaroxaban, aspirin, and other anticoagulants. These medications are often prescribed to patients with conditions like atrial fibrillation, deep vein thrombosis, or those at risk of a heart attack or stroke.
How Blood Thinners Work
Blood thinners work by interfering with the blood’s ability to clot. This process involves reducing the action of proteins or platelets that are necessary for clot formation. Doing so helps prevent existing clots from growing larger and stop new clots from forming, thus ensuring better blood flow and reducing the risk of serious health events.
Side Effects of Blood Thinners
While crucial for preventing blood clots, blood thinners can have several side effects. The most common and significant side effect is increased bleeding. This can manifest as nosebleeds, bleeding gums, heavy menstrual bleeding, prolonged bleeding from cuts, or unexpected bruising. In severe cases, it can lead to internal bleeding, which might not be immediately noticeable. Other potential side effects include dizziness, hair loss, rashes, and, in some cases, liver function abnormalities. Individuals on blood thinners should regularly monitor for signs of bleeding and discuss any unusual symptoms with their healthcare provider to manage these risks effectively.
When to Take a Blood Thinner
Blood thinners are typically prescribed in situations where your risk of blood clots is increased, which can lead to serious conditions like strokes, heart attacks, or pulmonary embolisms. Common scenarios for blood thinner use include:
- Certain surgeries, Such as knee or hip replacements, can increase the risk of blood clots due to decreased mobility.
- For heart and blood vessel diseases, including atrial fibrillation, where an irregular heart rhythm can lead to clot formation in the heart.
- If you have a history of clots: If you’ve previously had clots, especially deep vein thrombosis or pulmonary embolism, blood thinners help prevent recurrence.
- Following a stroke: To prevent additional strokes caused by blood clots in the brain.
The decision to start a blood thinner should always be made under the guidance of a healthcare professional. The professional can assess your individual risk factors and medical history to determine the appropriate timing and type of medication for your needs.
The Risks of Combining Blood Thinners and Alcohol
Increased Risk of Bleeding When
Alcohol consumption can significantly increase the risk of bleeding when combined with blood thinners. Alcohol affects the blood’s clotting ability and can amplify the anticoagulant effects of these medications. This heightened risk makes it easier for minor injuries to result in excessive bleeding, which can be particularly dangerous.
Impact on Blood Clotting
Alcohol can disrupt the balance of blood clotting, making it less effective at preventing blood clots and more prone to causing excessive bleeding. For individuals on blood thinners, this can mean a higher likelihood of both blood clots forming and uncontrolled bleeding occurring.
Interaction with Medications
Different blood thinners have unique interactions with alcohol. For example, warfarin and alcohol together can cause unpredictable changes in how the body processes the medication, leading to either too much or too little anticoagulation. Similarly, rivaroxaban and aspirin have their specific risks when mixed with alcohol. It’s essential to understand these interactions to avoid serious health complications.
Types of Blood Thinners and Their Interactions with Alcohol
Warfarin and Alcohol
Combining warfarin with alcohol can lead to increased bleeding risks and affect the medication’s efficiency. Warfarin requires careful monitoring, and adding alcohol into the mix can make it harder to maintain the correct dosage. It is generally recommended to limit alcohol consumption and always consult a healthcare provider for personalized advice.
Rivaroxaban and Alcohol
Rivaroxaban is another anticoagulant that can interact adversely with alcohol. Drinking alcohol while taking rivaroxaban can increase the likelihood of bleeding complications. Patients should follow their doctor’s guidelines regarding alcohol consumption to manage their health safely.
Aspirin and Alcohol
Aspirin is a common antiplatelet drug that can cause stomach bleeding when taken with alcohol. This combination can irritate the stomach lining, leading to ulcers or significant gastrointestinal bleeding. Following safe drinking practices and consulting with a healthcare provider is crucial.
Symptoms and Warning Signs of Complications
Signs of Increased Bleeding
When combining blood thinners with alcohol, it’s essential to watch for signs of increased bleeding. Symptoms may include unusual bruising, prolonged bleeding from cuts, blood in the urine or stools, and severe headaches or dizziness. If any of these symptoms occur, seek medical attention immediately.
Recognizing Alcohol Misuse
Alcohol misuse can complicate the use of blood thinners significantly. Signs of alcohol abuse include high tolerance to alcohol, inability to control drinking, and experiencing withdrawal symptoms when not drinking. Recognizing these signs is crucial for maintaining health while on blood thinners.

Safety Tips for Those Taking Blood Thinners and Consuming Alcohol
Consult Your Doctor
Before drinking alcohol while on blood thinners, it is vital to consult with your doctor. They can provide personalized advice based on your medication and overall health condition, ensuring you understand the risks and how to manage them.
Moderate Alcohol Consumption
If you choose to drink alcohol while on blood thinners, do so in moderation. Avoid excessive drinking and be aware of how much you are consuming. Moderation is key to minimizing risks.
Monitoring Health
Regular check-ups and monitoring are essential for anyone taking blood thinners and consuming alcohol. Keep track of any unusual symptoms and communicate with your healthcare provider to manage your health effectively.
Conclusion
Combining blood thinners with alcohol can lead to serious health risks, including increased bleeding and interactions with your medication. Understanding these risks and following safety guidelines can help manage these interactions. If you or a loved one is struggling with substance use and taking blood thinners, seeking professional help is crucial. Virtue Recovery Killeen offers comprehensive treatment and support. Call us today at 855-788-5582 to start your path to recovery.
FAQs
What are blood thinners and why are they prescribed?
Blood thinners are medications used to prevent blood clots and improve blood flow in individuals at risk of conditions like atrial fibrillation, heart attack, or stroke. They work by reducing the blood’s ability to clot, helping to prevent serious health events.
Can I drink alcohol while taking blood thinners?
Drinking alcohol while taking blood thinners can increase the risk of bleeding and affect the medication’s effectiveness. It’s important to consult your doctor for personalized advice and follow guidelines to ensure your safety.
What are the signs of complications from mixing blood thinners and alcohol?
Signs of complications include unusual bruising, prolonged bleeding, blood in the urine or stools, and severe headaches or dizziness. If you experience any of these symptoms, seek medical attention immediately.
What should I do if I suspect alcohol misuse while on blood thinners?
If you suspect alcohol misuse while on blood thinners, seek help immediately. Contact a healthcare provider or a treatment center like Virtue Recovery Killeen for support and guidance in managing your health and substance use.
Can you drink alcohol while taking Eliquis?
Drinking alcohol while taking Eliquis is not recommended as it can increase the risk of bleeding. Alcohol has anticoagulant properties that can enhance the effects of Eliquis, potentially leading to dangerous bleeding complications.
Can alcohol cause blood clots?
Moderate to heavy alcohol consumption can contribute to blood clot formation by affecting how the liver produces blood clotting factors. Additionally, alcohol-induced dehydration can thicken the blood, increasing the risk of clots.
Can alcohol withdrawal cause blood clots?
Alcohol withdrawal itself does not directly cause blood clots, but it can lead to a hypercoagulable state where the blood’s tendency to clot is increased. This risk is particularly elevated in individuals with chronic alcohol use disorder during the withdrawal phase.
Is Tylenol a blood thinner?
Tylenol (acetaminophen) is not classified as a blood thinner. It is an analgesic and antipyretic medication that does not significantly affect blood clotting mechanisms like some other over-the-counter pain relievers, such as aspirin.
Is it safe to drink alcohol with acne medicines?
Drinking alcohol while on certain acne medications, especially those that are systemic, like isotretinoin or tetracycline antibiotics, is not recommended. Alcohol can increase the risk of side effects like liver damage and can exacerbate dryness or irritation.
What fruits are natural blood thinners?
Berries, grapes, and citrus fruits are considered natural blood thinners due to their high content of salicylates and other compounds that can inhibit platelet aggregation. These fruits can help reduce blood clot formation and enhance circulation.
Can you drink coffee while on blood thinners?
Drinking coffee in moderate amounts while on blood thinners is generally considered safe, but it’s important to maintain consistency in your caffeine intake. Caffeine can affect the metabolism of certain blood thinners, such as warfarin, potentially altering their effectiveness. It’s advisable to discuss your specific situation with your healthcare provider to ensure that your coffee consumption doesn’t interfere with your medication regimen.
What happens when you mix blood thinners with alcohol?
Mixing blood thinners with alcohol can lead to several risky health complications. Alcohol itself has blood-thinning properties, and when consumed in conjunction with blood-thinning medications, it can significantly increase the risk of bleeding. This includes an elevated risk of internal bleeding, gastrointestinal bleeding, and bleeding in the brain, which are potentially life-threatening conditions.
Additionally, regular alcohol consumption can affect the liver’s ability to process certain blood thinners, particularly warfarin, leading to unpredictable medication levels and effectiveness. This can make it more challenging to maintain therapeutic drug levels, necessitating more frequent monitoring and adjustments by healthcare providers.
For these reasons, individuals taking blood thinners are usually advised to limit or avoid alcohol to manage their condition safely.
What are the Risks of Combining Ativan with Blood Thinners and Alcohol?
When combining Ativan with blood thinners and alcohol, there are serious risks that need to be considered. It’s important to ativan watch for symptoms healing, as the combination can increase the risk of excessive sedation, dizziness, and impaired coordination. This can lead to dangerous outcomes and should be avoided.
Resources
https://www.medicalnewstoday.com/articles/blood-thinners-and-alcohol
https://www.healthline.com/health/high-cholesterol/alcohol-blood-thinners-ate
https://www.drugs.com/article/bloodthinner-medications-alcohol.html
- About the Author
- Latest Posts
Nicki Lugo is currently employed as Clinical Director at Virtue Recovery Center in Las Vegas. Nicki is a licensed clinical professional counselor (CPC) in the state of Nevada and a licensed associate counselor (LAC) in the state of Arizona. She is also a licensed clinical alcohol and drug counselor (LCADC) in Nevada. Additionally, Nicki has specialized training in treating trauma and is a certified clinical trauma specialist (CCTS).
Nicki has earned a Master of Science degree in Psychology with an emphasis in Behavioral Health from the University of Phoenix and a Master of Science in Professional Counseling from Grand Canyon University. Currently, Nicki is pursuing a Doctor of Philosophy (PhD) in Counseling Education and Supervision at Grand Canyon University. Nicki’s research interests include the use of Positive Psychology interventions with dual diagnosis clients. Nicki hopes to contribute to the body of knowledge in treating substance use disorders.
Nicki’s long-term career goals include advancing in leadership roles within Virtue Recovery Center which is a quickly growing substance use disorder treatment facility. She hopes that one day her research and advocacy will help to save the lives of those who have been affected by substance use. She likes to say that advocacy is her passion and leadership is her superpower.